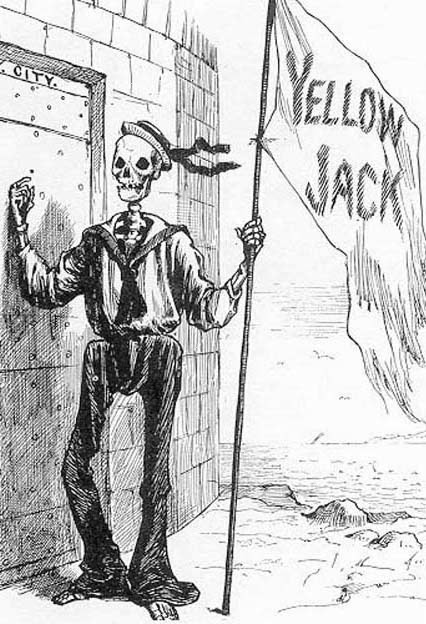
Yellow fever is a virus that is transmitted through two species of mosquito: Aedes and Haemagogus. Humans, however, can only get infected form the Aedes aegypti. These days, the disease is mainly found in certain countries in Africa and South-America, but it used to be more widespread, reaching all the way Europe and the Southern states in the USA.

Yellow fever has a wide range of symptoms, going from mild or asymptomatic to severe cases with haemorrhagic disease and organ failure. Yearly, 200,000 people get infected and 30,000 die. The disease has 3 stages: infection, remission and intoxication. Infection is the first stage, and can last between 3 and 6 days after receiving the infectious bite. Symptoms at stage 1 are very general, they include fever, headache, photophobia, backache etc. The disease then progresses to the remission stage, which last for a rather short time, between 12 and 48 hours, during which the symptoms go away and most people will recover. However, 15% of patients will continue on to the next stage of intoxication, where patients develop symptoms such as jaundice, oliguria or even worse anuria, haemorrhagic fever and multi-organ dysfunction. Patients that experience both multi-organ dysfunction and jaundice have a 50-80% chance of surviving. At the moment there is no treatment for yellow fever, alleviating the symptoms is the only possibility. Vaccination as a preventative measure remains therefore the best option.
The yellow fever vaccine is called YF 17D and is a live-attenuated vaccine. This means that YF 17D contains the yellow fever virus, but it has been treated so it won’t cause the disease. It takes 10-14 days after inoculation for the patient to be immune, so during that lag period is necessary to take precautions against the mosquito such as bed nets with insect repellent.
There are two main adverse events that the vaccine can cause, however, they are extremely rare.
The first is called vaccine-associated viscerotropic disease. The symptoms here are very similar to those of actual yellow fever, and this side effect can also result in death. However, this only occurs in 0.4 cases per 100,000 doses. Even though the chance of getting it is quite low, the fatality rate of this side effect is very high (63%). The vaccine is therefore only recommended to people living in yellow fever endemic countries and people travelling to those countries.
The second type of side effect is a range of neurological symptoms, such as meningoencephalitis, Guillain-Barré syndrome etc. These only occur in 0.8 cases per 100,000 doses and most people will recover from it.
For the past several months there has been a major outbreak of yellow fever in Africa, more specifically in Angola, the Democratic Republic of the Congo (DRC), and a separate outbreak in Uganda. The Angola-DRC outbreak has been particularly severe, with over 5,000 suspected cases and over 400 deaths in both countries. In order to contain the disease, mass vaccination campaigns are currently ongoing in these countries.
A global stockpile of emergency vaccines is kept, for exactly these sort of outbreak situations. Ensuring a swift response to curtail the epidemic. For yellow fever 6 million doses are kept as reserve, however, in the past 6 months a staggering 19 million doses were already administered and more are needed to protect the remaining population.
The problem that’s currently unfolding, is the time delay for vaccine production. It takes at least 6 months to produce a new batch of vaccines. In order to bridge this time delay, the WHO decided to administer only one fifth of the vaccine, in order to make the current supply last longer. A full dose of yellow fever vaccine allows gives lifelong immunity, one fifth of the dose covers people for a year. That should buy enough time to upscale vaccine production and hopefully contain the epidemic.
Gwendoline Deslyper
Minor PD. Live attenuated vaccines: Historical successes and current challenges. Virology. 2015;479-480:379-92. doi: 10.1016/j.virol.2015.03.032. PubMed PMID: 25864107.
Quaresma JA, Pagliari C, Medeiros DB, Duarte MI, Vasconcelos PF. Immunity and immune response, pathology and pathologic changes: progress and challenges in the immunopathology of yellow fever. Rev Med Virol. 2013;23(5):305-18. doi: 10.1002/rmv.1752. PubMed PMID: 23873723.
Miller ER, Moro PL, Cano M, Shimabukuro TT. Deaths following vaccination: What does the evidence show? Vaccine. 2015;33(29):3288-92. doi: 10.1016/j.vaccine.2015.05.023. PubMed PMID: 26004568; PubMed Central PMCID: PMCPMC4599698.
Messaoudi I, Basler CF. Immunological features underlying viral hemorrhagic fevers. Curr Opin Immunol. 2015;36:38-46. doi: 10.1016/j.coi.2015.06.003. PubMed PMID: 26163194; PubMed Central PMCID: PMCPMC4593727.
http://www.who.int/emergencies/yellow-fever/mediacentre/qa-fractional-dosing/en/
http://www.who.int/features/qa/yellow-fever/en/
http://www.who.int/mediacentre/news/releases/2013/yellow_fever_20130517/en/
http://www.cdc.gov/travel-training/local/HistoryEpidemiologyandVaccination/page27404.html
http://www.who.int/emergencies/yellow-fever/situation-reports/21-july-2016/en/
http://vaccine-safety-training.org/live-attenuated-vaccines.html